Optimize Front-End
Revenue Capture with AI
Billers rarely make billing errors. They occur before care begins through inaccurate intake, missed authorizations, or incomplete payer verification. Karma Health AI stops loss at the front.
Front-End Revenue Capture
Revenue leakage often starts before a claim is ever submitted. Incomplete patient data, misregistered insurance details, and missing authorizations are silent disruptors that lead to delayed payments and denied claims. For large healthcare networks, these front-end failures compound into measurable financial loss.
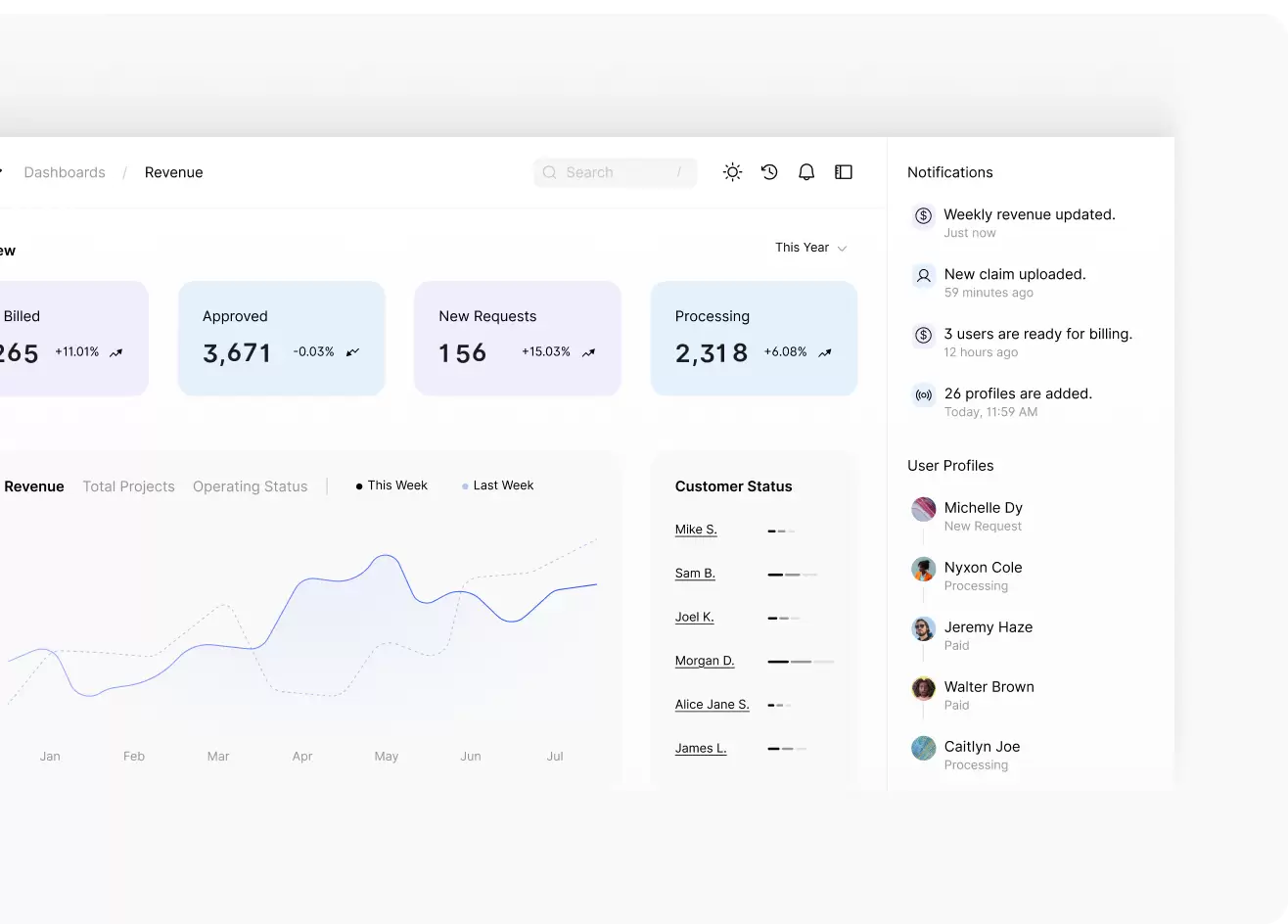
Karma Health AI brings clarity, speed, and precision to the front-end of your revenue cycle.
With our AI-enabled platform, you can:
- Validate demographic and insurance data at the point of registration
- Automate pre-service authorization workflows
- Identify high-risk payer policies before service
- Eliminate manual entry errors and downstream denial triggers.
AI-Powered Tools to Maximize Collections
Our AI platform continuously analyzes patient intake data, insurance details, and billing rules to flag discrepancies before they become denials. We reduce manual entry errors, missed eligibility verifications, and authorization gaps through intelligent automation.

Our proprietary systems use:
- Prevent claim rejections by identifying gaps at intake
- Accelerate coverage discovery and financial clearance
- Deliver tailored financial counseling based on the patient’s profile
- Reduce time to payment and avoid write-offs
According to Nellutla (2025), AI-powered registration tools reduce denial rates, improve scheduling efficiency, and increase revenue retention. Karma Health AI applies this intelligence to the front lines of billing, turning intake into an active revenue safeguard.
Front-End Revenue Capture for Streamlined Healthcare Finance
Fast-growing healthcare groups require finance systems that scale with growth. Front-end revenue intelligence does more than reduce denials; it aligns finance teams, providers, and administrators under a unified performance framework.
We support enterprise MSOs with:
- Seamless integration into EHR and practice management systems
- Real-time registration and eligibility dashboards
- Actionable denial prevention analytics
- Multi-location data normalization and performance benchmarking
Every dollar starts with clean data. Karma Health AI ensures it stays that way.
Front-End Accuracy Is Back-End Profit
Revenue loss is rarely the fault of back-office teams. Karma Health AI fortifies your first touchpoints, where data is captured, decisions are made, and revenue potential is secured or lost.

We will show you exactly how many opportunities you are missing, and how
Karma Health AI can help you capture them.
Frequently Asked Questions
What is front-end revenue capture?
Front-end revenue capture refers to processes at patient intake that directly impact billing, such as insurance verification, authorization checks, and data accuracy.
How does AI improve this process?
AI chronic disease management refers to using artificial intelligence to monitor, analyze, and support patients with long-term conditions. At Karma Health AI, this means using predictive models and real-time data to anticipate health risks and enable early, targeted interventions.
Can Karma Health AI integrate with my EHR and billing platform?
AI chronic disease management refers to using artificial intelligence to monitor, analyze, and support patients with long-term conditions. At Karma Health AI, this means using predictive models and real-time data to anticipate health risks and enable early, targeted interventions.
What results can I expect?
AI chronic disease management refers to using artificial intelligence to monitor, analyze, and support patients with long-term conditions. At Karma Health AI, this means using predictive models and real-time data to anticipate health risks and enable early, targeted interventions.
Is this solution scalable for multi-location groups?
AI chronic disease management refers to using artificial intelligence to monitor, analyze, and support patients with long-term conditions. At Karma Health AI, this means using predictive models and real-time data to anticipate health risks and enable early, targeted interventions.
